Basic Principles of the Law of Consent
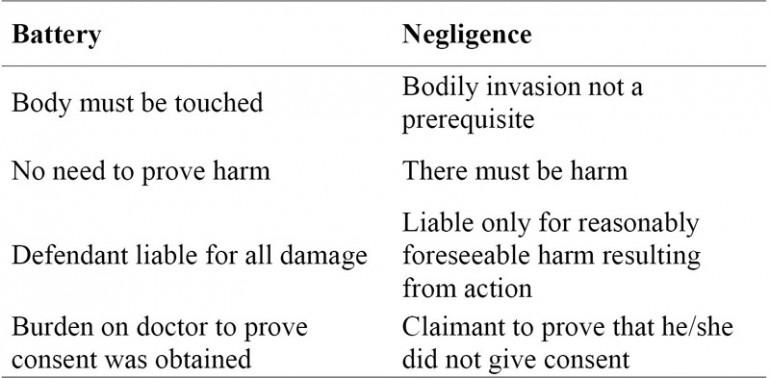
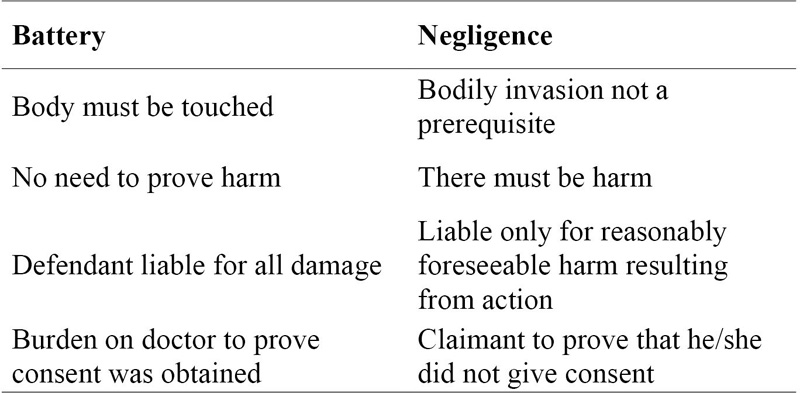
Chapter 3 Judges and legal scholars have long asserted the importance of patient autonomy in medical decision making. Yet autonomy has never been recognized as a legally protectable interest.1 In Chapter 2 an account was given of how developments in ethics and society at large progressively led to the erosion of paternalism and the ascendance (if not quite triumph) of the principle of self-determination. The mechanism by which this principle is protected in law is the law of consent, and legal developments have, in parallel with ethical and social developments, shaped our understanding of consent. In this chapter the basic principles of consent law are reviewed and an attempt is made to show how case law has responded to rapidly evolving ethical and social perspectives. The chapter sets the backdrop for the analysis that follows in later chapters. One of the earliest legal references to consent appears to be the 1767 case of Slater v. Baker and Stapleton where the courts imposed liability on a surgeon who failed to obtain consent.2 However, it was not until the twentieth century, starting with the US case of Schloendorff v. Society of New York Hospital, that legal cases on consent began to flourish.3 As more and more cases reached the courts, the law became more and more complex. Whereas the law at the time of Slater did not go beyond a requirement that the surgeon should not treat a patient without the patient’s authorisation, the law today requires the physician not just to obtain the patient’s assent but to provide sufficient information, seek to ensure that the patient understands, recognise quite specifically what the patient agrees to or does not agree to, respect any refusals and avoid a string of factors such as duress and deception which could vitiate consent.4 These requirements form the basis of the distinction that Faden and Beauchamp make between the legal and moral foundations of consent: The law’s approach springs from a pragmatic theory. Although the patient is granted a right to consent or refuse, the focus is on the physician, who holds a duty and who risks liability by failure to fulfil the duty. Moral philosophy’s approach springs from a principle of respect for autonomy that focuses on the patient or subject, who has a right to make an autonomous choice.5 In other words, the law’s approach to consent focuses heavily on the duties of the doctor, while ethics and moral philosophy focus more on the patient’s autonomous choice. The point has been made above that it is not pragmatic for the law to concern itself with whether a particular choice is autonomous; nevertheless, I will argue (see Chapter 9) that, if the patient’s right to self-determination is to be protected, the law should have this right as its starting point. In English law, a doctor undertaking treatment without consent may be liable for assault or battery or face an action in negligence.6 Battery and negligence are both torts; assault could be a crime. Battery is an intentional, unauthorised touching of another person, irrespective of whether any injury results and irrespective of whether or not the defendant acted in good faith.7 Assault is an intentional act which induces in the victim an apprehension of imminent harm or offensive contact, but the term ‘assault’ ‘is now, in both ordinary legal usage and in statutes, regularly used to cover both assault and battery’.8 In Scots law no distinction is made between assault and battery but this brief review of battery and negligence takes an English law perspective, as the key consent cases (Sidaway v. Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital9 and Chester v. Afshar10) informing the comparative analysis of the consent and property models (Chapter 9) are from the English jurisdiction. Although the English law perspective is taken, cases from other jurisdictions are cited where they help illustrate the various applications of the consent model. Assault is a common law crime if there was evil intent on the part of the perpetrator or recklessness in causing the victim to apprehend imminent violence.11 In relation to consent, doctors usually do not have the necessary evil intent, so there may be no criminal action, but they may face a civil action. For a civil law action there is no requirement to prove that the assault caused any damage, and the plaintiff only has to show that there was non-consensual touching.12 The doctor commits a trespass against the person (i.e. a battery or assault) if he/she treats that person without prior valid consent, whether or not his/her motive was hostile. This includes the situation where a doctor obtains consent from the patient to perform one type of treatment and subsequently performs a substantially different treatment for which consent was not obtained. This was what happened in the iconic US case of Mary Schloendorff, who was admitted into hospital in January 1908 for an examination under anaesthetic to assess the cause of her abdominal pain.13 While she was under anaesthetic, the surgeon removed a fibroid that had been found during the examination. There were post-operative complications and the patient sued the hospital. The case was decided in favour of the defendant at first instance and intermediate levels, and an appeal was heard at the state’s highest court, the Court of Appeal. This was where the judge made the following statement on consent, part of which is often quoted: In the case at hand, the wrong complained of is not merely negligence. It is trespass. Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault, for which he is liable in damages.14 (emphasis mine) In another case, a woman asked to be injected in her right arm but was injected in her left arm, and she won damages in battery.15 In another case that arose from a clerical error, the doctor was held liable in battery for operating on the patient’s back instead of a toe.16 An action in battery was successful when a woman who went in for a minor gynaecological operation suffered an injury to the womb and was sterilised.17 Examples from American jurisdictions where battery has been established as a consequence of consent being exceeded include consent given for a hernia operation but the doctor also removed both ovaries,18 myelogram19 involving a spinal puncture performed where consent had been for the simpler electromyogram20and a mastectomy being performed whereas the patient had only consented to exploratory surgery.21 In practice an action in battery is only brought when the doctor has deviated completely from the terms of consent, or where consent was obtained by misrepresentation (see below). Most consent cases take the form of an action in negligence, where the claimant seeks to establish that the defendant has breached a legal duty of care and that this breach has resulted in injury. Such a duty of care is presumed to be owed by a doctor to his/her patients, and this duty includes providing information.22 There are important differences between an action in negligence and an allegation of battery. Two differences relate to damage (harm). Negligence requires proof that the breach of duty (in this case, failure to inform) caused injury; in battery there is no need to prove that harm occurred. As Lord Scarman put it, ‘damage is the gist of the action in the tort of negligence’.23 Where harm occurs in battery, the defendant is liable for all damage that results from his or her action, while in negligence, the defendant is liable only for reasonably foreseeable harm.24 A further difference between battery and negligence in the context of consent is that a broad explanation of the treatment will usually be adequate defence to an allegation of battery, but more detailed discussion will usually be required in order to meet the duty of care in negligence.25 In Chatterton v. Gerson the claimant suffered numbness after a procedure to treat the chronic pain that she had in a scar.26 After a repeat procedure, also performed by Dr Gerson, she lost sensation in her right leg. Mrs Chatterton claimed trespass to the person in that there was no valid consent, since the implications of the procedures were not explained to her. She also claimed in negligence that the doctor had breached his duty of care by not providing sufficient information. Bristow J declared that ‘once the patient is informed in broad terms of the nature of the procedure which is intended, and gives her consent, that consent is real’27 and the cause of action for alleged failure to disclose risks is negligence, not trespass. Another difference is that by definition battery entails touching, so will not be applicable in consent cases (particularly refusal of treatment) where there has been no touching, whereas bodily invasion is not a prerequisite for establishing negligence. Truman v. Thomas exemplifies this difference.28 A woman who had repeatedly refused smear tests died of cervical cancer and her children sued the doctor for failing to warn her of the risks of not having this test. Such a case could not establish liability in battery as there was no touching, but could be brought in negligence as the duty of care mandates discussion of the risks and benefits of alternative treatments, including the alternative of no treatment. Thus, battery is inadequate for protection of patients’ choice in the vast and growing proportion of medical decision-making and treatment – for example, whether or not to take cholesterol-lowering medication – that does not entail physical contact. Lastly, in cases founded on battery, the onus lies on the doctor to prove that the patient consented to the treatment, whereas in negligence it is for the claimant patient to prove that he/she did not give a true consent.29 Table 3.1 Negligence distinguished from battery English courts have been reluctant to apply battery law in cases involving alleged non-disclosure of information to patients. In Sidaway, Lord Scarman specifically denounced as ‘deplorable’ the application of battery in claims for non-disclosure.30 By doing so, he endorsed the view expressed by Bristow J in Chatterton v. Gerson31 and Hirst J in Hills v. Porter.32 May J also considered such an action deplorable when he dismissed a claim in battery brought by persons who had been treated with human growth hormone (the Creutzfeldt-Jakob disease litigation).33 One reason why the courts have taken this position is that battery is an intentional tort. Cases of non-disclosure, even if negligent, are generally not the result of an intention to harm. Courts also consider it unfair to attach a stigma to doctors who have acted in good faith. Where there is evidence that the health-care professional did not act in good faith, however, the courts have not hesitated in finding him or her liable in battery. In Appleton and Others v. Garrett the claimants brought an action against an NHS dentist who, for fraudulent reasons, had grossly over-treated patients.34 Extensive treatment was carried out on teeth that were in pristine condition. He was found liable for battery. The court found that had the dentist properly explained the treatments and the need for them to the claimants they would not have consented to these treatments. All eight claimants were awarded aggravated damages for pain, suffering and loss of amenity. In some American jurisdictions, when a patient was not given prior warning of a potential complication (the occurrence of which was not an integral part of the treatment procedure but merely a known risk) and this risk materialised, the courts had tended to decide such cases in battery rather than negligence. Examples include failure to warn a patient a spinal operation involved an inherent risk of permanent paralysis35 and failure to warn of danger of radiation burns.36 The epochal judgment in Natanson v. Kline shifted the thrust from battery to negligence.37 Mrs Natanson suffered burns as a result of radiation therapy after mastectomy, and sued the radiologist, Dr Kline, for failing to warn of the nature and risks of the treatment. It was ruled that action relating to consent cases of this nature should be brought under negligence law rather than battery. An opportunity arose in Cobbs v. Grant for the California Supreme Court to clarify its position.38 Mr Cobbs’ spleen was ruptured during an operation for a duodenal ulcer in the hands of Dr Grant, and he needed a second operation to remove the spleen. Subsequently, he developed a gastric ulcer. Dr Grant had not warned him that the initial operation carried a 5 per cent chance of injury to the spleen and that the operation carried a chance of inducing other ulcers. Regarding the form of action to be brought in such cases, the court said: The battery theory should be reserved for those circumstances when a doctor performs an operation to which the patient has not consented. When the patient gives permission to perform one type of treatment and the doctor performs another, the requisite element of deliberate intent to deviate from the consent given is present. However, when the patient consents to certain treatment and the doctor performs that treatment but an undisclosed inherent complication with a low probability occurs, no intentional deviation from the consent given appears; rather, the doctor in obtaining consent may have failed to meet his due care duty to disclose pertinent information. In that situation the action should be pleaded in negligence.39 This exposition of the shift from battery to negligence is relevant because in Chapter 9 I will assess whether property analysis could either facilitate or inhibit a reversal of this shift. Although it is not currently fashionable for the tort of battery to be employed in the context of consent, it has been speculated that developments in human rights law could encourage the use of this avenue.40 Such speculation could be fuelled by academic commentators, like Kennedy who argued that: patients’ interests could well be better protected if the tort of battery were held to have a wider application. In particular, questions of what has come to be known as ‘informed consent’ could well be differently analysed and decided. A patient may have consented on the ‘nature and purpose’ test, but the information provided by the doctor may be so inadequate, in that it failed to respect the patient’s right to know, so as to be able to choose, that the consent should be regarded as entirely invalid. Such an extension to the tort of battery would restore the law’s protection of the symbolic harm represented by the complaint that the patient’s right to know was not respected. It would, in other words, reflect a response based upon rights.41 The goal of enabling patients to exercise their right of self-determination is handicapped by the narrow interpretation of consent in the tort of battery. Many years after Kennedy’s call for expansion of this tort, little has happened in this direction. Perhaps the key to unlocking this door is property analysis – we return to this in Chapter 9 where an argument is made for patient self-determination to be protected as a fundamental right, independent of any injury that may or may not result from infraction of this right. Meanwhile attention is focused on negligence, and in the rest of this chapter I discuss the requirements for valid consent, then the concept of informed consent. For consent to be valid the following must apply: a) The patient must have the capacity or competence to make the decision. b) There must be no undue influence. c) The patient must have been given [or offered] sufficient information about the proposed treatment.42 In theory each of these requirements is simple and clear enough. In practice, their application is more complex and, as discussed below, the courts have not always provided clear-cut and consistent guidance. In addition to these requirements which are cited in all standard descriptions of consent law and practice, one would add that there should be no misrepresentation. In Sidaway, Sir John Donaldson MR said that ‘if the consent is obtained by fraud or by misrepresentation of the nature of what is to be done … it can be said that an apparent consent is not a true consent’.43 In Salgo, Bray J. warned that ‘the physician may not minimise the known dangers of the procedure or operation in order to induce his patient’s request’.44 In R v. Tabassum it was held that consent to breast examination was vitiated by fraud, as the defendant had misled the women into believing that he was a doctor.45 In Appleton and Ors v. Garrett a dentist concealed information for financial gain and Dyson J. held that there was no valid consent (see above).46 The Bristol Inquiry recommended that where the procedure is experimental or innovative or the clinician inexperienced, the patient should be informed as part of the consent process.47 It is arguable that failure to comply with this recommendation could count as concealment of information for the personal gain of the doctor or hospital. As has been pointed out, competence ‘is not an all or nothing notion, as the legal definition suggests’.49 In clear-cut cases, where a patient is in a coma or severely mentally handicapped, he/she is clearly incompetent. At the other extreme is the highly knowledgeable and articulate patient with well-defined values and goals, who is able convincingly to communicate his/her wishes to the clinician. Most patients fall between the two extremes and determining competence to consent to a particular procedure is not always easy. The situation is compounded by the fact that a patient may be competent to give consent for one intervention but not for another. Strictly speaking a competent person must have a coherent set of beliefs that shapes his or her values or attitudes in a consistent way.50 In the absence of this coherent set of values, it is arguable that an authentic decision regarding medical treatment cannot be made. The assessment of competence is an onerous task for the clinician who must determine whether the patient is capable of retaining the information, weighing the options on balance against his or her values, beliefs and attitudes, and arriving at a decision.51 It has been observed that clinicians often do not proceed beyond a casual evaluation of patient competence due to time constraints, lack of communication and sometimes lack of education. On the other hand it is fair to say that a detailed assessment of competence is not necessary in all cases. An adult is presumed to be competent and a full assessment of competence is required only in those cases where the clinician has reason to rebut this presumption.52 For consent to be valid it must be given without undue influence.53 The Law Commission said that purported consent could be invalidated by ‘compulsion (that is physical force), coercive threats or offers (“duress”) and defective beliefs induced by fraud or mistake’.54 Coercion does not appear to be a major issue in clinical practice, but more subtle forms of undue influence are encountered. Tales of women who have been manipulated into having an unnecessary hysterectomy dramatically reflect ‘misinformed’ consent55 and it may well be that these extreme cases are the tip of an iceberg, with the less extreme or dramatic cases remaining hidden beneath the surface. The manipulation does not have to be ill-motivated for it to vitiate consent. A distinction is made between narrow and broad meanings of voluntary action, between truly volitional and constrained volitional actions.56 In the narrow definition of voluntary action, the subject simply exercises a choice between alternatives; in the broader meaning, the subject’s action is involuntary when his/her will is not taken away but his/her choice is unduly influenced. Take the case of a person who is held at gun point and opts to hand over his money rather than be shot. This is a choice he has made himself, but he is acting at the behest of the gun holder and does not have an independent reason for that action. He acted voluntarily in the narrow sense of the word but involuntarily in the broader sense – a constrained volitional action. In relation to patients’ decision-making in clinical practice, some decisions may appear to be volitional but are actually constrained volitional decisions. Health-care providers do not literally hold their patients at gun point, but in some situations (such as when submitting to an interventional procedure) a patient may not have an independent reason for taking a particular action and only does so in deference to the awesome figure of the medical establishment. The patient’s apparent agreement to the procedure in such situations has been said to be assent rather than consent but while this description makes a good point, it does not go far enough in capturing the patient’s captive situation. This type of agreement, which is common in medical practice, should be described as a constrained volitional agreement to treatment. Professional guidance57 on consent cautions against undue influence. In its guidance, the General Medical Council advises doctors: You must give information about risk in a balanced way. You should avoid bias, and you should explain the expected benefits as well as the potential burdens and risks of any proposed investigation or treatment.58 You must respect a patient’s decision to refuse an investigation or treatment, even if you think their decision is wrong or irrational. You should explain your concerns clearly to the patient and outline the possible consequences of their decision. You must not, however, put pressure on a patient to accept your advice.59 It is not always easy to determine where persuasion ends and undue influence begins. In Re T (Adult: Refusal of Medical Treatment) Lord Justice Butler-Sloss said that ‘[t]he degree of pressure to turn persuasion or appeals to affection into undue influence may be very little’,60 but in the same case Lord Donaldson said that it did not matter how strong the persuasion was, so long as it did not overbear the independence of the patient’s decision.61 The case involved a 34-year-old pregnant woman who, following a road traffic accident, developed a lung abscess and needed surgery but declined blood transfusion. Her mother was a Jehovah’s Witness but she herself was not one. Reversing the decision of the lower court, the Court of Appeal held that her refusal of blood transfusion was not binding on medical staff because her mother had unduly influenced her. Since the court agreed it was wholly acceptable that a patient should be persuaded by a third party so long as the final decision was the patient’s, health professionals should not be discouraged from using persuasion where necessary. The informational model of the doctor–patient relationship would not condone persuasion, but in Chapter 2 this model was discountenanced as being too consumerist and out of tune with medical professionalism. Persuasion is consistent with the collaborative model of the doctor–patient relationship and with medical beneficence; it also fits with the ecology paradigm underlying this book. The collaborative model obliges a doctor, for example, to try to persuade a patient to accept blood transfusion but such persuasion must not be allowed to degenerate into coercion. Faden and Beauchamp regard the use of persuasion as ‘an acceptable form of influence in informed consent contexts’.62 The courts, too, acknowledge that the doctor has a role beyond mere provision of options: … the patient, being unlearned in medical sciences, has an abject dependence upon and trust in his physician for the information upon which he relies during the decisional process, thus raising an obligation in the physician that transcends arms-length transactions.63 (emphasis mine) Undue influence could of course come from the patient’s family,64 but that is outside the scope of this analysis. The term ‘informed consent’ is frequently used in clinical practice and in the literature, and two authoritative books65 use the term in their title, despite the authors of one of the books recognising the term as a pleonasm.66 It is important to distinguish between ‘informed consent’ as a doctrine and ‘informed consent’ used imprecisely to mean a valid consent, one where the broad nature of the treatment proposed has been explained to the patient. This latter use of the term has been described as unhelpful since the requirement that consent be informed is only one of the ingredients of valid consent.67 It is arguable that the phrase is tautologous, as consent must always be informed if it is to be legally and ethically acceptable. In everyday life, people give meaningful consent (or assent) to various activities (e.g. agreeing to participate in a social activity) without having full information, but in legal usage, consent has to be informed in order to be valid. Jackson finds the term problematic because it is ambiguous, does not tell how much information should be provided, may make doctors over-burden patients with too much information and emphasises information provision at the expense of understanding.68 She expands on the ambiguity of the term as follows: … the expression ‘informed consent’ may be both ambiguous and misleading. It is, for example, commonly used as a convenient shorthand for two separate legal duties: the duty to obtain the patient’s consent before treatment, and the duty to ensure that the patient has been adequately informed about the risks and benefits of their therapeutic options. Nor is it clear whether the word ‘informed’ refers to the doctor’s behaviour or the patient’s state of mind. Is consent ‘informed’ if information has simply been provided before consent is given, regardless of whether the patient has in fact read, listened to, or understood anything? Or must the consent itself have been ‘informed’ by the patient’s prior consideration of all relevant material factors?69 Commentators from outside the UK have similarly criticised this term,70 and in this book it is used only when directly quoting other texts. The point (made rhetorically in the passage quoted above) about the importance of taking steps to check that the patient understands the information provided is revisited in Chapter 9. As a legal term, ‘informed consent’ refers to the doctrine, developed in the United States, which underlies the amount of information that a patient should be given in addition to the ‘broad nature’ of the treatment. Even when used in this sense, the term could be problematic and some commentators have avoided it, preferring terms such as ‘real’ or ‘meaningful’ consent,71 but other critics suggest that these alternatives are equally unhelpful to the extent that they ‘would render proof of causation still more difficult for claimants, and would enable doctors to justify non-disclosure on the basis of vague fears that the claimant was then incapable of making a sensible or rational decision’.72 This criticism, however, errs in assuming that ‘real’ or ‘meaningful’ implies ‘sensible’ or ‘rational’ consent. The phrase ‘informed consent’ originated in 1957 from amicus curiae submitted by the American College of Surgeons to the California Court of Appeals in Salgo v. Leland Stanford Jr. University Board of Trustees.73 Martin Salgo sued his doctors for negligently failing to warn him of the risk of paralysis resulting from translumbar aortography.74 The court sowed the seed75 of the doctrine of ‘informed consent’ when it held that the doctor owed a duty to the patient to disclose ‘any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment’.76 The seed of ‘informed consent’ germinated as a doctrine in Canterbury v. Spence, where it was held that it was for the court to determine the extent of, and any breach of, the doctor’s duty to inform.77 The claimant was a 19-year-old man with severe pain between his shoulder blades who was referred to a neurosurgeon. The doctor told him that he would have to undergo an operation (laminectomy) to correct a suspected ruptured disc. The patient did not object to the operation or ask any questions, but in answer to his mother’s question the doctor said the operation was not any more serious than any other operation. The day after the operation, the claimant fell from his hospital bed; he was paralysed in the lower half of his body and became permanently disabled. The claimant sued the doctor and hospital on the ground that the doctor was negligent in failing to disclose a risk of serious disability inherent in the procedure. In a landmark decision, Robinson J upheld the claim that the 1 per cent risk of paralysis should have been disclosed. Significantly, the court decided that the standard for determining whether adequate information had been given was not that of professional opinion but of the reasonable patient. In Sidaway, Lord Scarman summarised the doctrine as follows: … where there is a ‘real’ or ‘material’ risk inherent in the proposed operation (however competently and skilfully performed) the question whether and to what extent a patient should be warned before he gives his consent is to be answered not by reference to medical practice but by accepting as a matter of law that, subject to all proper exceptions (of which the court, not the profession, is the judge), a patient has a right to be informed of the risks inherent in the treatment which is proposed. The profession, it is said, should not be judge in its own cause; or, less emotively but more correctly, the courts should not allow medical opinion as to what is best for the patient to override the patient’s right to decide for himself whether he will submit to the treatment offered him.78 In a nutshell, the doctrine mandates full disclosure of material risks to the patient, and the standard of disclosure is to be determined not by the medical profession but by the court, taking account of the patient’s expectations. The full disclosure is not, however, referenced to the particular patient; it is full only in so far as it includes all that a hypothetical ‘reasonable patient’ would want to be told. The doctrine is American in origin and application, and Robertson suggests that expanding the liability of doctors was at the root of its development.79 As the key point of divergence or controversy between jurisdictions that embrace the doctrine and those that do not is the standard for assessing the quality and quantity of disclosure, this issue is addressed in more depth in the paragraphs below.
Basic Principles of the
Law of Consent
Should the Focus be on Patient or Doctor?
The Legal Development of Consent: Battery and Negligence
Differences between Battery and Negligence
Battery in Disclosure Cases: The Position of English Courts
Battery in Disclosure Cases: The Position in Other Jurisdictions
Resurgence of Battery?
Valid Consent
Competence48
Undue Influence
‘Informed Consent’ – the Term
Informed Consent – the Doctrine
Standards of Disclosure: What Constitutes Sufficient Information?