Tuberculosis Control and Directly Observed Therapy from the Public Health/Human Rights Perspective
Tuberculosis Control and Directly Observed Therapy from the Public Health/Human Rights Perspective
Introduction
The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being.
—Preamble to the WHO
Constitution UN, 1948
THE 1980s AND 1990s have seen a resurgence of interest in tuberculosis. Increasing cases world-wide led to the World Health Organization (WHO) declaring a global emergency in April 1993.1, 2 Despite the availability of ‘tools’ for controlling TB, programmes have been unable to sustain high cure rates.3 As a consequence of this, and the increasing problems of drug resistance, the international community, through the WHO, has developed and launched the directly observed therapy short course (DOTS) strategy.4, 5 This strategy is described as: government commitment to a national TB programme; case detection through ‘passive’ case finding (sputum smear microscopy for pulmonary tuberculosis suspects presenting at a health facility); short course chemotherapy for all smearpositive pulmonary TB cases (under direct observation for, at least, the initial phase of treatment [DOT]); regular, uninterrupted supply of all essential anti-TB drugs; and a monitoring system for programme supervision and evaluation.4–6
The DOTS strategy has achieved excellent results in New York and other parts of the US7–10 and in China.11 However, from other parts of the world voices have been raised asking if DOTS is the most effective way to control tuberculosis,12, 13 if DOTS can and should be perceived as a panacea,14 and if the DOTS strategy is ethical.15, 16
The control of infectious diseases like tuberculosis lies within the broad framework of public health. A currently accepted definition of public health is ‘providing the conditions in which people can be healthy’.17 Although public health contains within it many perspectives and disciplines, it is the biomedical perspective, the realm of medicine based on knowledge and practice from the natural sciences, which currently dominates thinking and approaches to health care and control of disease. Increasingly, it is being appreciated that biomedicine can benefit from working with other disciplines and perspectives. This interdisciplinarity encourages change and flexibility in approaches to health care and disease control.
A perspective which can complement and improve current approaches to the control of tuberculosis has been developed in recent years at the Harvard School of Public Health.18, 19 This approach looks at control of disease through the human rights framework, using the Declaration of Human Rights as a basis for analysing public health programmes.19 This framework enables a broader, more socially contextualised perspective on public health programmes. In this paper the current international strategy for tuberculosis control will be analysed using the health and human rights framework.
Background
Infectious Disease Control
Current public health control strategies are predominantly framed by the biomedical model and its associated methodologies.20 Of particular influence is public health’s core discipline, epidemiology, which, in investigating infectious diseases, looks primarily at interactions between ‘agent’, ‘host’ and ‘environment’. Interventions are designed to treat patients, ensure the protection of the population and prevent the occurrence of epidemics. The main strategies for control are to attack the source (e.g., treatment of cases/carriers of the isolation of cases); to interrupt transmission (e.g., environmental and personal hygiene, vector control); and to protect the susceptible population (e.g., immunisation, chemoprophylaxis).21
Tuberculosis Control
Current TB control strategies include the following components: case finding and treatment, chemoprophylaxis, vaccination with BCG and the improvement of socioeconomic conditions.22 The biomedical focus for TB control concentrates on reducing the transmission of pulmonary tuberculosis by targeting the most contagious persons (sputum-positive cases), by finding cases of sputum-positive TB and treating them until they become sputum-negative and are eventually cured.
Compliance
Compliance is an important part of TB control and can be defined as the extent to which a person’s health-related behaviour coincides with medical advice.23 It can be a problem for many infectious disease control programmes. The direct observation of treatment (DOT) contained within the DOTS strategy is designed to enhance patient compliance. The strategy requires that the patient take his or her medications in the presence of a health care worker or other ‘responsible’ third party. In the biomedical/public health terms described above, DOT is part of the strategy for ‘attacking the source’ of infection and rendering the person non-infectious by treating him/her with the appropriate drugs for an appropriate period of time. DOT is fast becoming the standard approach for control of many infectious diseases, including sexually transmitted diseases, leprosy and tuberculosis.16 Nevertheless, recent observers have noted that the intervention may be ethically problematic.16 Embedded within it is the imbalance of power and capacity between the public health profession and the infected person. An uncritical application of DOT may also create problems by placing the onus for cure on the patient, while masking the responsibility of the health care professionals and health care structures to ‘provide the conditions in which people can be healthy’.16 Others have acknowledged the shared obligations of the patient in the need to comply with biomedical treatment, and of society in the need to provide the patient with the necessary treatment facilities.24, 25
Sumartojo has recently called for the development of an approach to improving compliance which engages with the responsibility of health care structures to provide an appropriate service and which ‘… recognise(s) the needs and dignity of patients’.26 Similarly, Farmer has noted that ‘[t]hroughout the world, those least likely to comply are those least able to comply … these settings are crying out for measures to improve the quality of care, not the quality of patients’.27
Potential Problems with the DOTS Strategy
The increasing use of DOT in infectious disease programmes and the development of the DOTS strategy for TB control have coincided with a reappraisal (in some quarters) of the principles underlying public health interventions.16, 28, 29 Also under renewed consideration is the need to understand the interaction and balance between the health needs of the individual and the health needs of the society. The kinds of questions being asked are: Is public health too paternalistic? Is there an imbalance of power and capacity between the public health profession and the infected person? If so, are these imbalances being reinforced by public health control measures? Are there alternative ways of approaching public health interventions that would redress, rather than reinforce, these kinds of imbalances and inequalities?15, 20, 24
Human Rights and Public Health: A Framework for Negotiation
Human Rights
In 1948 the Universal Declaration of Human Rights was accepted and adopted by the participating members of the United Nations.30, 31 Today these principles continue to be relevant, and are being applied to considerations of health. It has recently been suggested, for example, that the extent to which human rights are realised may represent a better and more comprehensive index of well-being than traditional health status indicators.18 From a public health perspective, while the availability of medical and other health care constitutes one of the essential conditions for health, the availability of these technologies and services does not in itself create ‘health’. Indeed only a small fraction of health status variations between populations can be attributed to health care: clearly, then, adequate health care32 is a necessary, though not sufficient, constituent of health.
The Health and Human Rights Analysis
Public health and human rights can be considered as two complementary, though often conflicting, ways of looking at human well-being. Even when they address similar, or even identical problems their language and underlying assumptions differ. Public health, for example, is built on the principle of seeking the greatest good for the greatest number of people: health is important and public health is considered a valid reason for limiting individual rights under some circumstances. The principles on which the human rights discourse is based, on the other hand, are concerned with promoting the well-being of individuals by ensuring respect for their rights and dignity. Interweaving these perspectives, then, it becomes clear that public health aims and interventions must be the least intrusive and least restrictive measures available to accomplish the public health goal.19 Any ensuing compromise of an individual’s rights must apply equally to all those affected.
In order to explore, negotiate and debate the potential tensions between human rights and public health policies, programmes and practices an approach known as the Health And Human Rights Framework has been developed.33 The framework can be used to analyse public health programmes in order to provide ‘new’ ways of intervening which embrace both of these two complementary, but again sometimes conflicting, ways of looking at health issues.
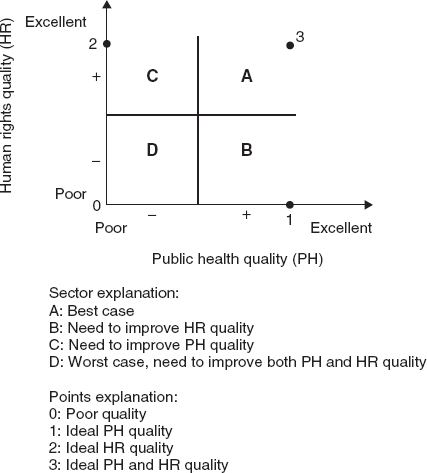
The framework involves: 1) assessing the extent to which the proposed policy or programme represents ‘good public health’; 2) discerning whether the proposed policy or programme is respectful and protective of human rights; 3) finding how the best possible combination of public health and human rights quality can be achieved; and finally 4) asking if the proposed policy or programme still appears to be the optimal approach to the public health problem (Figure 38.1).33 To ensure that the full range of potential burdens on human rights is identified, each of the rights listed in the Universal Declaration of Human Rights should be considered.33
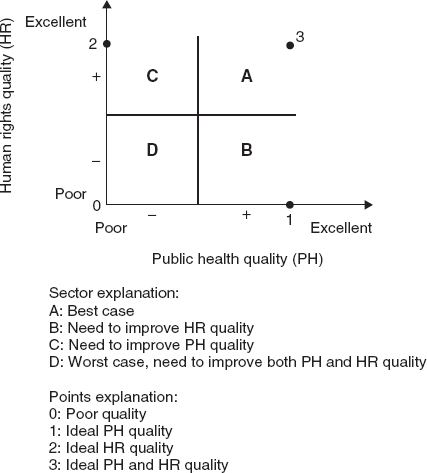
Figure 38.1 A framework for negotiation: human rights and public health. (Reproduced with kind permission from AIDS, Health and Human Rights, the International Federation of Red Cross and Red Crescent Societies, and Francois-Xavier Bagnoud Center for Health & Human Rights, Harvard School of Public Health, Boston, 1995.)
Tuberculosis Control from a Human Rights Perspective
To What Extent Does the Proposed Policy or Programme Represent ‘Good Public Health’?
As already stated, public health strategies for the control of infections concentrate on disease rather than ‘well-being’. From a biomedical perspective, TB control strategies are ‘rational’ approaches developed from good science. As only people with sputum-positive pulmonary tuberculosis are regarded as being infectious to others, and because control needs to prevent transmission to the wider public, public health interventions are targeted at cases of infectious TB only (primarily sputum-positive pulmonary tuberculosis). Forms of TB that are considered non-infectious, such as extrapulmonary TB or TB in children, are not, therefore, seen to be public health issues. While ‘rational’ from a positivist, biomedical point of view, the human rights approach would question this perspective. What message does this give to the parents of children with tuberculosis? What message does it give to people with extra-pulmonary disease?
There is an inherent contradiction in the public health approach to the control of infectious diseases like tuberculosis. While the interest of a programme is ultimately the good of the population, the strategy focuses on the individual patient, who is treated without reference to the social conditions that frame his or her life. Take, for example, a TB programme that simply focuses on the act of directly observing patients take their medication, without taking into account the economic and social factors that are associated with the disease. A patient in this situation may be forced to discontinue treatment because a) she cannot travel to the clinic every other day for DOT, either because she lacks resources herself or because her household has refused to support her; b) she may not be able to tell her family that she has TB (and therefore cannot ask for support) because a TB diagnosis may precipitate divorce or obviate her marriage chances; c) she is feeling too unwell to travel the sometimes long distances over difficult roads; and/or d) she simply cannot afford to take the time out of daily life (work, responsibilities for child care, etc.). Such a programme is unlikely to achieve the hoped for results. Barnhoorn and Adriaanse note that before the obstacles to a particular treatment regimen can be cleared away, patients have to understand the system, and the system must be consistent with the underlying health beliefs and social norms of the community.34 The programme will also need to take account of the practical realities of everyday life which play a role in the ability of people to adhere to any treatment regimen.
Is the Proposed Policy or Programme Respectful and Protective of Human Rights?
In reviewing the human rights articles from the perspective of current TB control activities, several broad concepts will be considered: stigma, treatment, adherence to medication, limitations of freedom, education and living conditions. Seeing TB control from a different perspective and addressing these issues with greater sensitivity will lead to better care of TB patients.
Stigma