Mental Health and Inequity: A Human Rights Approach to Inequality, Discrimination and Mental Disability
Introduction
On October 3, 2008, The Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act was signed into law in the United States. This legislation introduced parity for mental health coverage for the first time in large group health insurance plans.1 Theoretically, this brought an end to a system in which it was legal for insurers to limit care for mental health and substance abuse conditions and to require patients to pay more out-of-pocket costs than are required for other medical conditions.2 The Act has been hailed as a progressive step toward removing inequities in access to and affordability of mental health care. At a political and public level, this may reassure those who live with serious mental disabilities and those who campaign for equality. The reality, however, is that the significant array of parity provisions at both the state and national levels constitute a major barrier for service users and clinicians in realizing real equality as an outcome of this legislation. The Act allows health insurers to determine which mental health and substance use conditions they will cover, to define for what conditions coverage is “medically necessary,” and to gain exemption from the law if providing mental health and substance use coverage increases their costs by 2% or more in the first year or by 1% or more in subsequent years. Furthermore, as Richard G. Frank, a health economist at Harvard Medical School, has observed, people with serious mental disabilities such as schizophrenia require many services, including psychosocial and occupational rehabilitation services, which are crucial to their recovery but are not provided for by the Act.3
Thus, legislation may be enacted to reduce or eradicate inequalities in health care, but statutes on their own often introduce only “formal equality”—that is, the law treats all individuals or health conditions alike. This is a superficial and deceptive form of equality, however, as there are many social, economic, and political factors at play that obstruct the translation of a law into the real, individual experience of equality. Formal equality alone gives an illusion that all are equal and that fairness exists, without addressing underlying inequalities in power, access, and socioeconomic and political circumstances.4 In this way, formal equality alone tends to perpetuate discrimination and inequality because it often fails to address real inequality in circumstances. Under a seemingly progressive veneer of respectability, disparities grow unchecked as public advocacy groups relax their activist efforts. Thus, far from bringing about progressive change, the introduction of equality legislation can have reactionary effects, exacerbating existing disparities in health access and care.
Within the human rights framework, it is imperative that we strive to achieve “substantive equality,” defined here as equality of opportunity, within the context of structural inequalities present in society. This means that circumstances that prevent the individual from achieving equality of opportunity must be addressed and that barriers to access and empowerment must be removed. Within health care, substantive equality does not guarantee equality of treatment outcomes, but it does guarantee equality of opportunity in trying to achieve those best outcomes.5
Mental disability and mental health care are surprisingly overlooked within the global discourse on health equality, and mental health has always appeared to be a side issue in both the public and academic health debate.6 There appears to be social distaste for issues pertaining to mental health and disability.
A significant exception to this attitude was the adoption of the United Nations Convention on the Rights of Persons with Disabilities on December 13, 2006.7 The Convention was negotiated during eight sessions of an Ad Hoc Committee of the General Assembly from 2002 to 2006. To date, there have been 140 signatories to the Convention (with 59 ratifications) and 83 signatories to the Optional Protocol (with 37 ratifications). The Convention is intended as a human rights instrument with an explicit social development dimension:
It marks a “paradigm shift” in attitudes and approaches … from viewing persons with disabilities as “objects” of charity, medical treatment and social protection towards viewing [them] as “subjects” with rights, who are capable of claiming those rights and making decisions for their lives based on their free and informed consent as well as being active members of society.8
The Convention is broadly inclusive in terms of what is defined as disability, stating that “[p]ersons with disabilities include those who have long-term physical, mental, intellectual or sensory impairments which in interaction with various barriers may hinder their full and effective participation in society on an equal basis with others.”9 Thus, the Convention constitutes a significant global commitment to a human rights framework in which issues of achieving substantive equality and the full and unfettered rights of persons with disabilities are placed at center-stage.
The importance of this Convention (as well as that of other recent regional declarations on mental disability) cannot be underestimated; mental disabilities are pervasive, common, and responsible for a significant proportion of disability, suffering, mortality, and lost productivity in human society. The social and economic “burden” borne by individuals, their families, their communities, and nations due to mental disability is enormous.10 Co-morbidity with physical illness and substance abuse is considerable.11 The relationship between mental disability and poverty, income inequality, social dislocation and alienation, and homelessness is well supported by growing evidence.12 Mental disability impacts education, social behavior, economic productivity, and cultural norms. Moreover, in the treatment of such conditions as HIV/AIDS and drug-resistant tuberculosis, mental disability is associated with high-risk behavior, poor treatment adherence, and inability to access care. In short, mental disability is a protean phenomenon whose often hidden tentacles extend into multiple areas of human experience and functioning. And yet, in both high-income countries (HICs) and lowand middle-income countries (LMICs) throughout the world, mental health care is a low priority, receiving stunted budgets, inadequate resources, and little attention from government.13 Globally, the integration of mental health into primary care is still in its infancy, while the skills, knowledge, and confidence of generalist health practitioners in managing mental disability are pitiful.14 In most countries, the level of mental health and substance use education and knowledge within the general public is minimal, if not negligible. Inequalities in mental health service development, provision, and access exist at all levels and in different contexts.15
The care, treatment, rehabilitation, and full integration of persons with mental disabilities is a complex challenge that cannot be met through the narrow confines of a purely biomedical or even public health model. The social, economic, cultural, and political factors that interact with innate and acquired biological processes in the genesis, course, and outcome of mental disabilities cannot be ignored in striving for equality. Efforts to improve global mental health will fail dismally if they are limited to the development of new drugs and therapeutic interventions. Likewise, attaining full human rights for persons with mental disabilities will never be achieved through a reliance on public health system reform alone.
Importantly, a human rights approach to mental disability requires a paradigm shift, as the Convention articulates, away from a public health approach in its conventional sense. A public health approach is inadequate, as it serves to reinforce paternalism and charity in identifying mental disability as a medical issue necessitating a medical “solution.” It views mental disability as a health issue only, requiring a health services response. In contrast, a rights-based approach to mental disability means acknowledging the social, economic, and political forces that result in the disability experienced by people with impairments. It also means ensuring that the principle of participation, as well as leadership by persons with disability in advocacy for substantive equality, is key to any international or domestic efforts to redress the inequalities and discrimination that exist in society. For health professionals involved in efforts to achieve real equality, a clinical role alone is ineffective. Instead, clinical expertise must be complemented by a commitment to an activist agenda in partnership with persons with mental disabilities—an agenda focused on bringing about change to the structural inequalities within social, economic, and political life that prejudice mental health, promote social exclusion, and retard recovery from mental disability.
Terminology and Models of Mental Disability
The institutionalized medical language of mental disability is, at best, pejorative and situates mental conditions squarely within an individual disease framework. Terms such as “mental disease” and “mental disorder” construct psychological, emotional, and behavioral conditions as innate, biological, pathological states independent of socioeconomic, cultural, and political context. Likewise, the prevailing medical model of mental disability—which defines disability as an individual’s “restriction in the ability to perform tasks” and handicap as “the social disadvantage that could be associated with either impairment and/or disability”—serves to establish a direct causal relationship between individual impairment and disability.16 In contrast, the social model of disability, theorized by disabled activist and scholar Michael Oliver, views disability as something imposed upon persons by an oppressive and discriminating social and institutional structure and that is over and above their impairment.17
While the social model has characterized the disability movement and has been adopted as a basis for a human rights approach to disability, it is not beyond critique. For example, the British medical sociologist, Michael Bury, adheres to what he calls a sociomedical model of disability in which he reaffirms the reality of impairment in contributing to disability.18 In addressing the “causality” of mental disability, I am inclined to agree with Bury. Research has largely discredited a strict social model view of the causality of serious mental disability associated with such conditions as schizophrenia and bipolar illness to instead support a significant role for genetic and other biological factors in conferring vulnerability to these conditions. Importantly, this integrated, or multifactorial, view of the genesis of mental disability does not support the traditional medical or individual model either. In other words, a critique of the social model does not imply a return to the strict medical model that it superseded. Instead, what is consistent with current evidence from both the biological and sociological fields of research is a model of mental disability that integrates biological and social (as well as cultural and political) factors in establishing cause for these conditions.
The concept of “impairment” is not straightforward here. In terms of mental disabilities, impairment cannot be understood as a fixed structural or mechanical “abnormality” or “departure from human normality,” as Lorella Terzi expresses it.19 Innate or acquired genetic or biological factors associated with the origins of serious mental disabilities are not fixed impairments in the sense that blindness and spinal paralysis are. Rather, these factors exist as “vulnerability factors”—rendering the individual susceptible to psychosocial and environmental factors within society. Structural environmental forces act in concert with innate or acquired vulnerability factors over time to give rise to illness and disability. Complex reciprocal gene–environment interactions throughout neurodevelopment, involving both environmental mediation of gene expression and genetic influence over individual responses to environmental stressors, lie at the heart of most mental disabilities.20
Multiple Levels of Inequality and Discrimination
A rights-based approach to mental disability needs to be informed by a clear analysis of the multiple levels of inequality and discrimination that exist in relation to individuals with mental disabilities both within and outside the health system. In a sense then, a “situation analysis” is required to illustrate the clear links that exist among social, economic, political, and cultural aspects of the environment and the origin, personal experience, and outcome of mental disabilities. The following discussion details how substantive inequality and discrimination characterize the manifestation and experience of mental disability in society as well as the provision of mental health care. While this analysis is intended to have global relevance, it contains an overrepresentation of data from the United States. This is not because that nation is alone in experiencing the inequalities cited, but rather, it is a reflection of the fact that significant research has been conducted in this field within the US, while there is a relative paucity of evidence available from other countries.
Unequal Prevalence Due to Structural Inequalities
In recent years it has become apparent that the prevalence of a number of mental disabilities varies in relation to social and economic disparities within societies. For example, systematic reviews show differences in both the prevalence and incidence of schizophrenia in relation to variables including urban versus rural status, social class, migration, unemployment, homelessness, and income inequality.21 In the case of schizophrenia, social and economic factors mediate expression of the condition in biologically vulnerable individuals.22 Such is the extent to which these factors impact negatively upon both the onset and outcome of schizophrenia that Brendan Kelly has invoked Paul Farmer’s concept of “structural violence” in relation to this illness.23 Kelly argues that social, economic, and political factors such as poverty and income inequality “shape both the landscape of risk for developing [schizophrenia] and the context in which health-care is provided.”24 He maintains that these forces constitute a form of “structural violence” that impacts the development and course of schizophrenic illness. Common mental disabilities such as anxiety, depression, and substance abuse also show an increased prevalence in relation to social class, unemployment, low income, homelessness, poverty, and income inequality.25 This means that individuals, families, and communities that occupy lower social classes, that are experiencing high levels of unemployment, and that are living in poverty also bear the burden of increased risk for mental disability along with all of its associated consequences. With respect to income inequality, it appears that health depends not just on personal income but also on the incomes of others in the society.26 While individual rank within the income distribution is undoubtedly important, it is clear that a large rich–poor gap within a community is bad for everyone in that community regardless of rank, not just for those at the bottom.
Unequal Service Access Due to Structural Inequalities
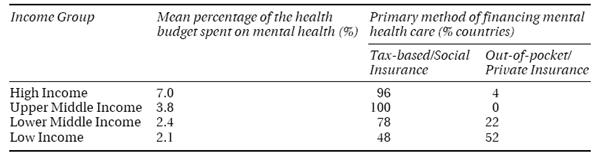
Social and economic factors may serve as barriers to accessing mental health services in high-income countries as well as low- and middle-income countries. A community survey in the US (a high-income country), for example, reported that low-income individuals cited financial barriers to accessing care. However, this was not the case in the Netherlands or in Canada, both HICs, where economic disparities and income inequality are lower.27 Also in the US, a household survey of adolescents found that those of low-income status reported far more structural barriers to accessing mental health services than did their middle- and high-income counterparts.28 In LMICs, the impact of socioeconomic factors is likely to be greater.
The “treatment gap” (that is, the absolute difference between prevalence and percentage treated) for mental disabilities is significant worldwide and is due to a number of factors, including lack of knowledge about mental disabilities, stigma, lack of service availability, and socioeconomic barriers to accessing available services.29 An earlier study in Belize, for example, reported that 63% of individuals with schizophrenia, 89% of individuals with affective conditions, and 99% of individuals with anxiety conditions were untreated.30 The World Health Organization Mental Health Survey conducted in 14 countries found that 76–85% of individuals with serious mental disabilities in LMICs received no treatment, while 35–50% of those in HICs received treatment.31 Clearly, lack of treatment cannot be attributed solely to socioeconomic barriers to access—other likely reasons have already been mentioned. However, within LMICs like South Africa, it is patently obvious that poverty, disempowerment, and inadequate health education impede access to care. In such countries with high poverty and unemployment rates, those in need often cannot afford medical fees, the medicines prescribed, or the transport to convey them to clinics and hospitals. In such contexts, it is glaringly apparent how social and economic inequities lead to inequalities in access to care.
Unequal Service Access Due to Race, Ethnicity, and Gender
Racial and ethnic minorities in the United States are discriminated against in terms of their access to mental health services and appropriate treatments.32 Margarita Alegría and colleagues reported that of those who had depressive disorder in the previous year, more African Americans (59%), Latinos (64%), and Asians (69%) received no mental health treatment for depression compared with non-Latino whites (40%), while Daniel Rosen and colleagues found that nearly a quarter of white women (23%) with a mental disability received treatment as opposed to only 9% of African American women.33 In a sample of patients with schizophrenia living in the community, Richard Van Dorn and colleagues reported that significantly fewer African American patients had received atypical antipsychotics (the preferred therapy) than their white counterparts.34 Disparities in access to mental health services also exist with regard to gender. Women of low socioeconomic status have been shown to be at particular disadvantage in accessing mental health care, and there are clear barriers to accessing alcohol and substance abuse services for women compared with men.35